Table of Contents
Colon cancer, one of the most common cancers worldwide, often develops silently in its early stages. Recognizing symptoms and understanding risk factors can be life-saving. Also known as colorectal cancer, it is a disease that affects the large intestine (colon) or rectum. It’s a significant health concern, but understanding its symptoms, risk factors, and available treatments can make a real difference. This blog post provides valuable information about colon cancer, presented clearly and accessibly.
A Brief History of Colon Cancer:
While the exact origins of colon cancer in humans are difficult to pinpoint, evidence of cancer-like diseases exists in ancient civilizations. Modern understanding and diagnosis of colon cancer have evolved significantly over time.
- Early Observations: Ancient Egyptian and Greek writings mention ailments potentially linked to colorectal issues.
- 18th and 19th Centuries: As medical knowledge advanced, anatomical understanding of the digestive system improved, leading to more accurate descriptions of colon and rectal cancers. Surgical techniques also began to develop.
- 20th Century: Major strides were made in diagnostic tools like colonoscopy and imaging techniques. Radiation therapy and chemotherapy emerged as treatment options. Research into the genetic basis of colon cancer also began.
- 21st Century: We continue to see advancements in early detection through screening programs, more targeted therapies, and a growing understanding of the role of lifestyle factors in colon cancer development.
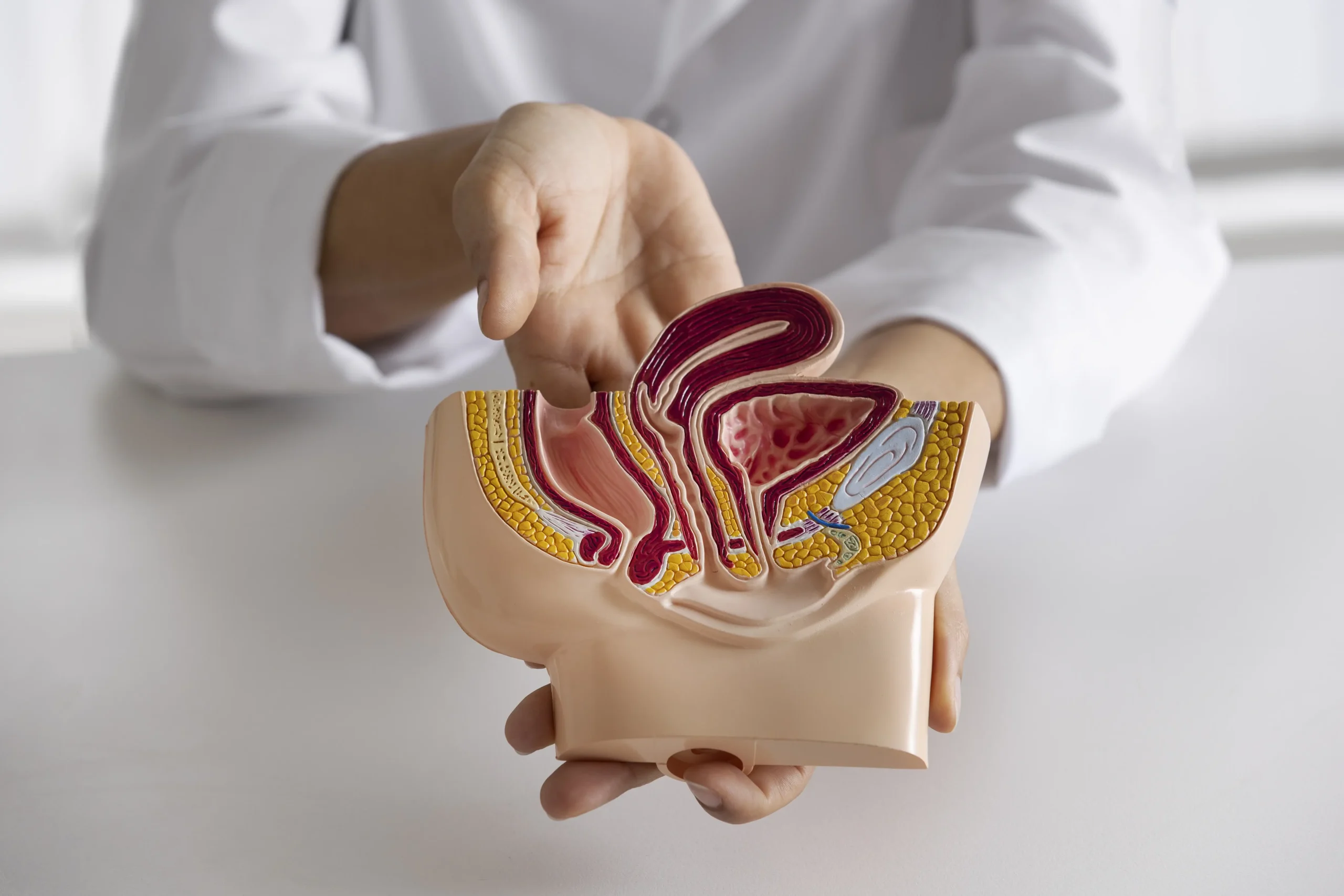
How Colon Cancer Starts:
Colon cancer usually begins as small, benign (non-cancerous) growths called polyps on the inner lining of the colon or rectum. Over time, some of these polyps can become cancerous. Genetic mutations play a significant role in this transformation. While some mutations are inherited, others are acquired during a person’s lifetime due to factors like lifestyle, diet, and environmental exposures.
Key Risk Factors:
Some risks are unavoidable, while others can be managed:
- Age: Risk increases after 50, though younger adults are increasingly diagnosed.
- Family History: Genetic syndromes (e.g., Lynch syndrome) or relatives with colon cancer.
- Inflammatory Bowel Disease (IBD): Crohn’s disease or ulcerative colitis.
- Lifestyle Factors:
- Diets high in processed/red meats and low in fiber.
- Sedentary habits, obesity, smoking, or heavy alcohol use.
Colon Cancer Symptoms:
Early-stage colon cancer often has no noticeable symptoms. This is why regular screening is so important. However, as the cancer progresses, some common symptoms may appear:
- Changes in bowel habits: This can include diarrhea, constipation, or a change in the consistency of your stool (narrow or ribbon-like).
- Rectal bleeding or blood in your stool: This is a significant warning sign and should never be ignored. The blood can be bright red or darker.
- Persistent abdominal discomfort: This may involve cramps, gas, bloating, or pain.
- A feeling that your bowel doesn’t empty completely: Even after a bowel movement, you might feel the urge to go again.
- Unexplained weight loss: Losing weight without trying can be a sign of an underlying health issue.
- Fatigue or weakness: Feeling unusually tired, even after rest, could be a symptom.
- Anemia: A low red blood cell count can be detected through blood tests and can cause fatigue and weakness.
It’s important to remember: These symptoms can also be caused by other conditions. If you experience any of these symptoms, it’s crucial to consult your doctor for proper evaluation and diagnosis. Don’t self-diagnose!
When to See a Doctor?
Don’t wait if you experience:
- Blood in your stool (visible or detected in a lab test).
- Symptoms lasting longer than 2–3 weeks.
- Unexplained fatigue, weight loss, or anemia.
- A family history of colon cancer or polyps.
- Sudden, severe changes in bowel patterns.
Early detection saves lives: Over 90% of cases are treatable when caught early.
Treatments:
The treatment for colon cancer depends on several factors, including the stage of the cancer, its location, and your overall health. Common treatments include:
- Surgery: Often the primary treatment, surgery aims to remove the cancerous tissue.
- Chemotherapy: Drugs are used to kill cancer cells. Chemotherapy may be used before or after surgery, or to treat advanced cancer.
- Radiation therapy: High-energy rays are used to target and destroy cancer cells. Radiation may be used before surgery to shrink a tumor or after surgery to kill any remaining cancer cells.
- Targeted therapy: These drugs attack specific vulnerabilities in cancer cells.
- Immunotherapy: This treatment helps your immune system fight cancer.
Frequently Asked Questions (FAQs):
Q: How is colon cancer diagnosed? A: Colonoscopy is the most common diagnostic test. During a colonoscopy, a flexible tube with a camera is inserted into the rectum to examine the colon. Biopsies can be taken during a colonoscopy to test for cancer. Other tests, like stool tests and imaging scans, may also be used.
Q: Who is at risk for colon cancer? A: Several factors can increase your risk, including age (risk increases after 50), family history of colon cancer, personal history of inflammatory bowel disease, certain genetic syndromes, smoking, excessive alcohol consumption, obesity, physical inactivity, and a diet high in red and processed meats and low in fruits and vegetables.
Q: Can colon cancer be prevented? A: While not all cases can be prevented, you can reduce your risk by:
- Getting regular screening tests.
- Maintaining a healthy weight.
- Eating a diet rich in fruits, vegetables, and whole grains.
- Limiting red and processed meat consumption.
- Exercising regularly.
- Not smoking.
- Limiting alcohol intake.
Q: What is the survival rate for colon cancer? A: The survival rate varies depending on the stage of the cancer at diagnosis. Early detection significantly improves the chances of successful treatment and survival.
Q: Blood in Stool: Is It a Sign of Colon Cancer?
Yes, blood in the stool (hematochezia) can be a sign of colon cancer, but it’s crucial to understand that it can also be caused by many other conditions. These include hemorrhoids, anal fissures, diverticular disease, inflammatory bowel disease (IBD), and other gastrointestinal issues.
- How it relates to colon cancer: Blood in the stool can occur when a tumor in the colon or rectum bleeds. The blood may be bright red if the tumor is in the lower part of the colon or rectum, or it may be darker and mixed in with the stool if the tumor is higher up in the colon.
- When to see a doctor: Never ignore blood in your stool. It’s essential to see a doctor to determine the cause, even if you suspect it’s something benign like hemorrhoids. Early diagnosis of colon cancer significantly improves treatment outcomes.
Source: The American Society of Colon and Rectal Surgeons (ASCRS) emphasizes the importance of seeing a doctor for any rectal bleeding. Their website provides patient education materials on colorectal conditions. (https://fascrs.org/) The National Cancer Institute (NCI) also lists rectal bleeding as a possible symptom of colorectal cancer. (https://www.cancer.gov/)
Q: Changes in Bowel Habits: A Colon Cancer Symptom?
Changes in bowel habits, such as diarrhea, constipation, or a change in the consistency of your stool (narrow or ribbon-like stools), can be a sign of colon cancer, especially if these changes are persistent. However, like blood in the stool, these changes can also be caused by other factors, including diet, stress, infections, and irritable bowel syndrome (IBS).
- How it relates to colon cancer: A tumor in the colon can obstruct or irritate the bowel, leading to changes in bowel habits.
- When to see a doctor: If you experience persistent changes in your bowel habits, especially if they are accompanied by other symptoms like blood in the stool or abdominal pain, it is essential to consult your doctor.
Source: The Mayo Clinic lists changes in bowel habits as a symptom of colon cancer. (https://www.mayoclinic.org/) The American Cancer Society (ACS) also includes this information in their materials about colorectal cancer. (https://www.cancer.org/)
Q: Unexplained Weight Loss: Could It Be Colon Cancer?
Unexplained weight loss, meaning losing weight without actively trying to do so, can be a sign of colon cancer, although it’s more often associated with more advanced stages of the disease. It’s also a symptom of many other medical conditions, including other cancers, thyroid problems, and depression.
- How it relates to colon cancer: Cancer cells can use up a lot of energy, leading to weight loss. Also, a tumor can affect appetite and nutrient absorption.
- When to see a doctor: If you experience significant and unexplained weight loss, it’s essential to see your doctor to determine the cause.
Source: The NCI mentions unexplained weight loss as a possible sign of cancer in general, including colorectal cancer. (https://www.cancer.gov/)
Q: Abdominal Pain and Colon Cancer: What You Should Know
Abdominal pain, including cramps, gas, bloating, or a general ache, can be a symptom of colon cancer. However, abdominal pain is very common and has many causes, most of which are not serious. These include gas, indigestion, and muscle strains.
- How it relates to colon cancer: A tumor can cause pain by obstructing the bowel or by pressing on nearby organs.
- When to see a doctor: If your abdominal pain is severe, persistent, or accompanied by other symptoms like blood in the stool or changes in bowel habits, it’s essential to see a doctor.
Source: The Cleveland Clinic lists abdominal pain or cramping as a possible symptom of colon cancer. (https://my.clevelandclinic.org/)
Q: Fatigue and Colon Cancer: Is There a Connection?
Fatigue, feeling unusually tired even after rest, can be a symptom of colon cancer. However, it’s a very general symptom with numerous potential causes, including lack of sleep, stress, depression, anemia, and other medical conditions.
- How it relates to colon cancer: Cancer can cause fatigue through various mechanisms, including anemia (low red blood cell count), inflammation, and the production of substances that affect energy levels.
- When to see a doctor: If you experience persistent and unexplained fatigue, especially if it’s accompanied by other symptoms, it’s essential to consult with your doctor.
Source: The ACS includes fatigue in its list of general cancer symptoms. (https://www.cancer.org/) The NCI also discusses cancer-related fatigue. (https://www.cancer.gov/)